Answers About Fentanyl Lethality and Overdose Potential
Struggling with a fentanyl addiction is a life-threatening condition and can be extremely dangerous. More so than even opioid addiction. Illicit fentanyl has become much more common on the street and it has caused overdoses to skyrocket. But how does fentanyl kill you, exactly?
Despite the dangers, there are ways to address a fentanyl addiction and get the help that you need.
I entered Best Rehabs In Arizona for treatment after multiple overdoses and coming as close to death as one can with fentanyl. Drug abuse is a brutal condition to combat, but dealing with a drug like fentanyl requires a whole different level of addiction treatment.
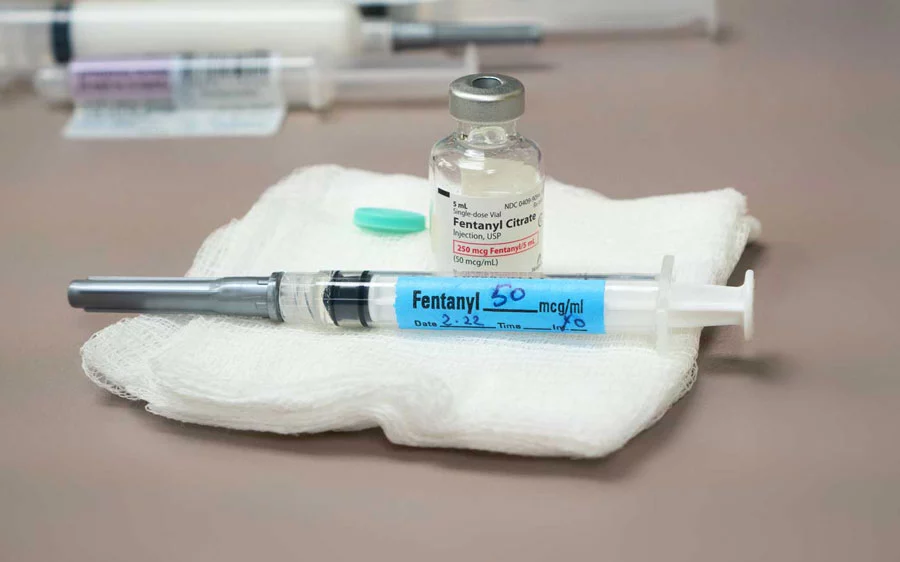
Pharmaceutical fentanyl and illicit fentanyl are both deadly and can be abused just like any other drugs. With the rise of opioid abuse in this country, drug dealers have found new ways to cut these drugs, and fentanyl typically is used in this process. A lot of people who ingest fentanyl don’t even realize they are taking such a deadly drug.
Keep reading to find answers to how does fentanyl kill you, and how Best Rehabs In Arizona Recovery can offer you the same sort of foundation for sobriety that I found with their help.
The Rise Of Fentanyl Use and Fentanyl Overdoses
How long fentanyl stays in your system depends on your level of addiction and your body mass. Pharmaceutical fentanyl in pill form can take minutes before you feel the effects, while a fentanyl patch can one to two days to take effect. Fentanyl is usually only prescribed to people with severe pain associated with cancer and other extreme illnesses.
Many drug tests don’t detect fentanyl, and a separate test may be required to detect it. With a drug that’s manufactured to treat severe pain, it’s no wonder that when taken recreationally it can be dangerous. Because it’s used to treat chronic pain, it is easily abused. According to the Drug Enforcement Administration, Fentanyl is a synthetic opioid that is fifty to one hundred times more powerful than morphine.
Because of the rise of fentanyl, many addiction treatment programs are designed to treat that specific addiction. Because fentanyl is such a potent synthetic opioid, intervening in a fentanyl addiction is a life or death situation. The world of drug abuse changes over time, and new substances make their way onto the market all the time. No one has ever seen anything like the rise of fentanyl.
Fentanyl Withdrawal Symptoms

A fentanyl withdrawal is very similar to opiate withdrawal symptoms. Fentanyl withdrawal symptoms include flu-like symptoms, muscle aches, nausea and vomiting, and respiratory changes. These withdrawal symptoms vary in severity depending on a multitude of factors. Fentanyl withdrawal symptoms can persist for up to two weeks.
Plenty of other drugs come with very uncomfortable withdrawal symptoms, but opioids and synthetic opioids like fentanyl are particularly rough. I used heroin for a number of years and dabbled here and there with fentanyl. Even though I knew how dangerous it was, my fentanyl abuse continued and led me down the darkest path I’ve ever been down.
My fentanyl use messed with every part of my body. My liver function was affected, and I suffered from respiratory depression and shallow breathing. Even heavy users of opioids don’t experience the difficulty that fentanyl abuse causes. When I began taking fentanyl, my body was already in a rough spot because of my heroin abuse.
How To Detect Fentanyl Through Drug Tests
Fentanyl has led to new developments in drug testing technology. Fentanyl test strips are a way to test for fentanyl and can tell you how long fentanyl can stay in your system. Fentanyl is not easily detected in urine tests, hair tests, or saliva tests. Fentanyl test strips have revolutionized the way that we test for fentanyl.
Before my fentanyl abuse, I dealt with long-lasting opioid dependence. My drug use began in my early twenties and continued until I was in my late thirties. Even though I was a substance abuse veteran, nothing could prepare me for what fentanyl did to me. Powder fentanyl is what I became addicted to, but it didn’t start there.
My first experience with fentanyl was through counterfeit pills. These are fentanyl-laced prescription drugs that are very much responsible for the rise in overdose deaths associated with this drug. It’s extremely difficult to prevent people from ingesting these pills, because, on the black market, drug users are going to do what they’re going to do.
Fentanyl can come in many different forms. There is the powder form, but there are also nasal sprays and a transdermal patch. Fentanyl powder can also be cooked down into an injectable solution. There aren’t many other substances that come in so many different forms.
When To Seek Help

Even though I was able to hide my addiction from my loved ones, it was eating me alive inside. I suffer from a variety of mental health disorders, namely bipolar depression. This was very tricky when it came time for me to seek help. I had a lot of issues to work through beyond just my substance use.
Because I had such a severe addiction, I needed medical supervision during my detox. Getting fentanyl out of a person’s system takes a rather brutal detox process. Anyone who has been addicted to any powerful opioid will tell you how uncomfortable it is to ween yourself off of it. The side effects are crushing and can make you want to give in very easily.
When I entered rehab, I was facing potential prison time because of where my drug addiction took me. Every drug test they gave me through probation I would fail. I was given a lot of chances, but the drug testing always told the truth. I couldn’t be trusted to get help on my own.
How Does Fentanyl Kill You?
There’s no handbook for how to overcome an addiction to fentanyl. I never imagined that addiction treatment would do anything for me. Because I was so highly addicted, it seemed like it would take an act of god for me to not go back to my old ways. Drugs stay in your system longer the more you take them. It took nearly three weeks after my last dose for the drug’s half-life to dissipate.
When I finally took the last drug test that showed that I had rid of the drug from my body, it was a unique feeling. It felt like there would always be something that would come back. When you’ve quit using the drug and it still shows up in standard drug tests, it can feel like it will never go away.
There are a lot of things that got me through that initial phase of recovery. The behavioral therapies I engaged in were extremely helpful, and all the other recovering addicts I’ve met along the way have helped me stay the course. Using fentanyl as long as I did made me realize how damaged my body and my soul had become. No matter how much damage is done, you can always heal.
How To Overcome Such A Highly Addictive Drug

I got used to taking drug test after drug test when I was a fentanyl addict. Through probation and jail, I was given every type of drug test you could imagine. After taking so many blood tests, urine tests, and the occasional hair test, it really makes you feel like a human experiment.
Now that I am clean, I have a much different appreciation for forensic medicine. All of the advances in drug testing and screening for other opioids have saved many lives. I consider myself a part of this process as well as I continued my sobriety journey. I’ve met all kinds of people through group therapy who have inspired me.
These groups are a wonderful collection of folks who have overcome many different addictions, from opioids to alcohol. A lot of these people are at many different stages of their recovery as well. Some of these people are still close enough to the beginning of recovery that they still experience withdrawal symptoms. The best thing that I can do is be there to support them and let them know they aren’t alone.
Finding Lasting Recovery From Fentanyl
Individual therapy as well as family therapy has worked wonders for me in my sobriety. Gone are the days when I would pray before drug tests, hoping nothing would be detected in my urine. The respiratory arrest, insomnia, and body chills are no longer there. I am no longer looking up on the internet how I can beat a drug test. I am no longer searching for how does fentanyl kill you, as I found out firsthand.
When I go to meetings, I bring a positive attitude with me. I focus on solution-based thinking as opposed to problem-based thinking. I am no longer all doom and gloom in my personal life. It’s been a long road, but I have traveled it willingly and am open to addressing whatever issues may arise in the future.
Put Worries About Drug Testing in Your Past
I am open and willing to talk about my struggle and am aware that I’m not invincible to it. I can still slip up and go back to my old routine of using drugs, getting in trouble, and being subjected to hair tests and saliva tests. Fentanyl will stay with me forever, but in a different way than it used to.
If you are struggling with fentanyl, give yourself a chance at sobriety with the program for recovery found at Best Rehabs In Arizona. They helped me, and I am willing to bet they will give you solid options for a different outlook on life as well!